Is Neurofeedback Evidence Based?
Neurofeedback for ADHD: What the Science Really Says
Introduction
ADHD is one of the most common struggles for kids and adults today. People with ADHD often have trouble focusing, sitting still, or thinking things through before acting. While medication and therapy can help, not everyone responds well to those options. That’s why more and more families and professionals are asking: what else is out there? One answer that keeps coming up is neurofeedback.
Neurofeedback is a brain-based therapy that’s been around for decades but has only recently started gaining serious attention. Some people say it works wonders, while others call it a waste of time and money. So what’s the truth? Is neurofeedback actually backed by science? Or is it just hype?
In this blog, we’ll walk through the facts. We’ll explain what neurofeedback is, why it’s being used for ADHD, and what the research says—especially two big studies that have shaped the conversation. We’ll also look at why some experts still aren’t convinced, and what that means for families and professionals trying to make the best decisions.
By the end, you’ll understand both sides of the debate and why many believe the hesitation around neurofeedback isn’t because it doesn’t work—but because people just don’t know enough about it yet.
What Is Neurofeedback?
Think of neurofeedback as “brain training.” During a session, sensors are placed on the person’s head to measure brainwave activity. This information is shown in real time through a computer program—usually as a simple video game or animation. When the brain does something helpful (like becoming more focused or calm), the game responds positively—maybe the screen gets brighter, or a rocket ship moves forward. When the brain gets off track, the feedback stops. Over time, the brain learns how to stay in those better patterns.
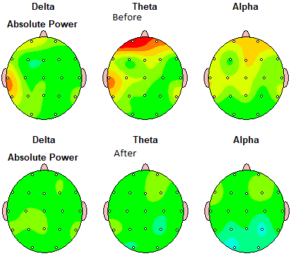
Neurofeedback is based on the idea that people with ADHD often have brainwave patterns that are out of balance—usually too much of the slow “daydreamy” activity (theta waves), and not enough of the faster, focus-related activity (beta waves). By rewarding the brain for shifting toward more balanced patterns, neurofeedback aims to improve focus, reduce impulsivity, and help regulate energy levels.
There are a few main types of neurofeedback used for ADHD:
- Theta/Beta Training: Helps reduce daydreaming (theta) and increase focus (beta)
- SMR Training: Targets physical stillness and calm attention
- SCP Training: Teaches the brain to shift into a more alert or relaxed state on command
These approaches are the most researched and have the best track record in clinical studies.
The Big Picture: Two Major Research Reviews
To understand why people say neurofeedback is (or isn’t) evidence-based, we need to look at two important research reviews—called meta-analyses. These studies combine results from many smaller studies to see what the overall data shows. Let’s break down the findings of each.
- Arns et al. (2009): Early Strong Support
In 2009, a group of researchers led by Martijn Arns looked at 15 studies on neurofeedback for ADHD. They found that neurofeedback led to large improvements in attention and impulsivity, and moderate improvements in hyperactivity. The results were strongest in studies that used common protocols like theta/beta and SMR training.
They also pointed out that some studies used “sham” or fake neurofeedback (where the person got random feedback instead of brain-based feedback) and real neurofeedback still came out ahead. This helped show that the improvements weren’t just from placebo or therapist attention.
The authors concluded that neurofeedback met the highest level of scientific support at the time—calling it “efficacious and specific.” In other words, not only did it work, but it worked because of the brain training itself—not just because kids were being paid attention to.
- Van Doren et al. (2020): It Lasts
Fast forward to 2020. Another team of researchers wanted to know if the benefits of neurofeedback actually lasted over time. They analyzed 10 randomized studies that included follow-up ratings months after treatment ended.
Here’s what they found:
- Neurofeedback improvements held up over time—and even got stronger in some areas. Kids who did neurofeedback continued to improve in attention and self-control, even after the training stopped.
- Compared to kids who got no treatment, the neurofeedback group was doing significantly better six months later.
- Compared to medication, neurofeedback worked a bit more slowly, but had similar long-term effects—and without the side effects or need to keep taking a pill.
The takeaway? Neurofeedback isn’t just a short-term fix. It can lead to lasting changes in the brain and behavior, which makes it a great option for people looking for long-term solutions.
So Why Is Neurofeedback Still Controversial?
If neurofeedback has this much positive research, why are some professionals still unsure about it? There are a few reasons.
- Not All Neurofeedback Is the Same
Neurofeedback isn’t one single method. There are different protocols, different technologies, and different levels of training among providers. Some clinics use well-researched approaches; others might use newer or experimental techniques that haven’t been proven yet. That makes it hard to compare all the studies or make one-size-fits-all recommendations.
For example, the strongest evidence supports the protocols mentioned earlier (theta/beta, SMR, SCP). But when studies include other, less-tested approaches, the average results aren’t as strong. It’s kind of like lumping all “therapy” together—some types work better than others depending on the person and the problem.
- Questions About Placebo
Some experts argue that the improvements seen with neurofeedback could be due to placebo effects—especially when parents or kids know they’re getting a fancy new treatment. That’s why recent studies have tried using “sham” neurofeedback to test this.
In a few of those studies, both the real and sham groups improved right after treatment, which suggests that expectations do play a role. But in the months that followed, only the real neurofeedback group kept getting better—suggesting there’s more going on than just placebo.
Still, this is one of the biggest debates in the field. More sham-controlled studies are needed to put the question to rest.
- It’s Not Taught in School
Most doctors, therapists, and school staff never learn about neurofeedback in their training. That means they may not be familiar with the research, or may only have heard of it from secondhand sources. And as with anything new or unfamiliar, it’s easy to be skeptical.
Once professionals actually see how neurofeedback works and how the results play out in real life, many change their minds. But getting to that point requires more awareness and education.
- Standardization and Training Vary
Unlike medications, which are mass-produced and regulated, neurofeedback is a skill that depends on the provider’s training and the tools they use. While there are certifications and guidelines, not every provider follows them. That can lead to mixed results—and frustration if someone doesn’t see improvement.
The good news is that more and more providers are following best practices and using evidence-based protocols. As the field continues to grow, standardization is improving.
What We Know Today
Despite the debate, there are some clear takeaways:
- Neurofeedback works best when using the right protocols and done by a trained provider
- It’s especially helpful for improving attention and impulse control
- The benefits last over time, even months after treatment ends
- It’s safe, non-invasive, and doesn’t rely on medication
It may not work for everyone, but neither do meds or therapy. For families looking for something that teaches the brain how to stay calm and focused—rather than just managing symptoms day-to-day—neurofeedback is a real option.
Final Thoughts: A Shift in Thinking
Neurofeedback isn’t magic. It’s a tool that uses learning and repetition to help the brain work better. And while it might not be right for every person or every situation, the science shows it can make a real difference for many people with ADHD.
The main thing holding it back right now isn’t a lack of results—it’s a lack of awareness. The more people learn what neurofeedback really is, and how it’s been studied, the more it moves from “alternative” to “accepted.”
If you’re a parent, case manager, or clinician thinking about neurofeedback, the key is to find a provider who uses evidence-based protocols, tracks progress, and explains the process clearly. And remember—just because something isn’t well known yet doesn’t mean it isn’t worth exploring.
The brain is always learning. Neurofeedback just gives it the feedback it needs to learn how to perform better.
If you, or someone you love, is struggling with migraines and you’re looking for a natural ADHD treatment, get in touch with us for a free consultation to learn more about neurofeedback and how it is an effective, non-invasive, drug-free ADHD treatment.


